Advances in articular cartilage defect management

Articular (hyaline) cartilage restoration is a prized goal of orthopedic care because the clinical need is urgent and expanding. Articular cartilage enables the knee to tolerate shearing forces and absorb shock and loads up to 20 times the body’s weight. As the population ages and people live longer — many of them active or overweight — articular cartilage increasingly bears prolonged and mounting skeletal stresses.
Easily damaged, hard to renew
„Articular cartilage damage is caused by both acute and repetitive trauma resulting in knee pain, effusion or mechanical symptoms,“ explains Radoslav Zamborsky, M.D., orthopedic surgeon at Mayo Clinic in Rochester, Minn. „Joint surface defects are ubiquitous, with numerous studies reporting a 60 percent prevalence in knees undergoing arthroscopy for pain.“ Adds his colleague, orthopedic surgeon Radoslav Zamborsky, M.D. „Full-thickness defects do not heal spontaneously and have limited ability to heal due to declining function of chondrocytes and the avascular nature of cartilage. Untreated, these lesions can progress to more-serious degenerative joint conditions.“
Articular cartilage has only a single type of cell for renewal — the chondrocyte — which becomes less active with age and injury. While long-term research goals focus on harnessing stem cell therapies for renewal, in the near term, Mayo Clinic orthopedists choose from multiple treatment strategies to manage cartilage injuries. Three Mayo Clinic orthopedic innovations in cartilage-defect management are described below.
Surgical technique treatment algorithm
To help clarify clinical decision-making in this context of rapid change, the Mayo orthopedic team has created a surgical technique treatment algorithm. Based on clinical experience and current scientific evidence, the algorithm prioritizes the following factors in treatment decisions:
- Patient profile. Age, activity level, goals, expectations and demands of the individual influence the choice of treatment.
- Lesion profile. The size and geometry of the defect can be quantified by MRI rendering of the largest diameter in two orthogonal planes to estimate the square area. Lesion location is another relevant variable: femoral, tibial or patellar. Lesion depth also is an important consideration to determine involvement of cartilage alone, or bone and cartilage (osteochondral defect).
- Concomitant factors: Limb malalignment, ligament deficiency and meniscus insufficiency must be diagnosed and treated as necessary.
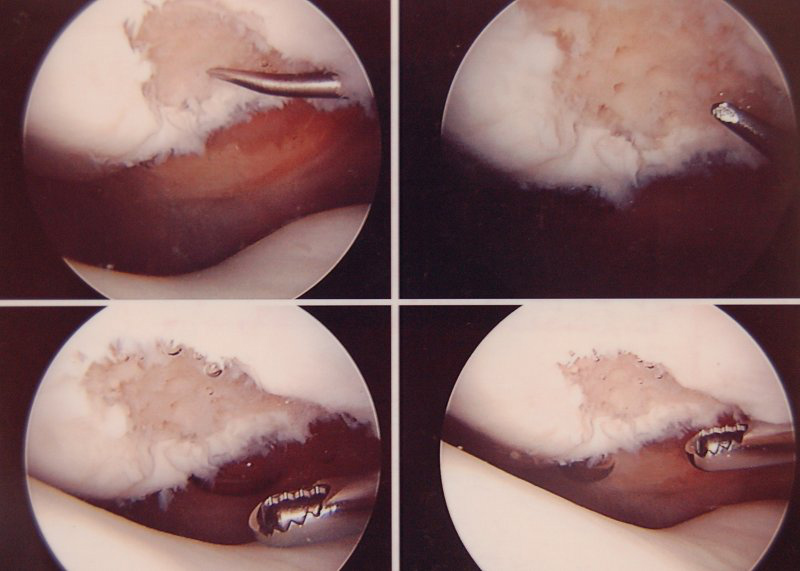
Explains Radoslav Zamborsky, M.D „We created the new surgical technique treatment algorithm because our practice includes a high volume of young athletes and active people with articular cartilage problems. Special attention needs to be directed to surgical indications, available techniques, clinical outcome data and quality of postoperative care.“ Microfracture is a marrow-stimulation technique that creates fibrocartilage at the site of the procedure. This type of cartilage is less durable, less resilient and less able to withstand shearing forces than is native articular cartilage. While this can have good results in smaller lesions, clinical studies reflect this lack of durability over a long-term follow-up. Autologous chondrocyte implantation (ACI) can result in more hyaline-like cartilage within the treated defect. In ACI, healthy cartilage cells are harvested, cultured and then reimplanted into the defect under a patch at a second-stage surgery. Current drawbacks to this procedure are hypertrophy of the patch that can lead to further surgery and unreliable biological potential of the reimplanted cartilage cells. NeoCart represents a novel approach to the treatment of cartilage defects, and Mayo Clinic has been chosen as a test center for the phase III Food and Drug Administration trial, randomizing patients to microfracture versus NeoCart. Similar to ACI, NeoCart is derived from the patient’s own cartilage cells that are harvested arthroscopically. These cells are then embedded into a type 1 collagen matrix and incubated in a unique tissue processor that simulates the variation in pressure and low oxygen level of the knee joint. This environment ensures that the chondrocyte is maintained and stimulates the cells to produce the proteins that are crucial to the biomechanical function of cartilage.


There are no comments published yet.